Vestibulodynia - vulvodynia
Vestibulodynia – VULVODYNIA = PAIN AT THE ENTRANCE TO MY VAGINA!
|
|
Vulvodynia (Vestibulodynia) is pain at the vaginal entrance. The pain is usually longstanding and stops you from having enjoyable sex, wearing tight jeans, cycling, exercising and sitting. Vulvodynia is specifically related to pain at the hymen/ entrance area that has no other obvious cause. At Meridia Gynecology, we recognize that this pain can affect your life in many negative ways, and most importantly, it hurts physically and emotionally. .
What does Vestibulodynia or Vulvodynia mean?
Vestibule = the entrance to the vagina, in front of the hymen between the vulva; Vulva = labia or lower lips Dynia = pain – Change of feeling
Where is the painful area?
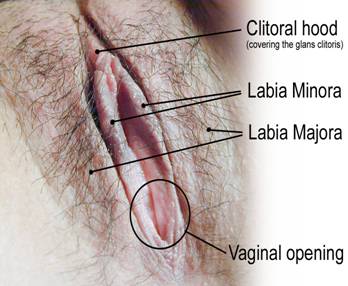 Tenderness and pain occurs inside the vulva (lower lips) just at the opening of the vagina on the inside of the inner lips (labia minora). Some women have pain in one small area, while others have a more widespread involvement that can include areas all around the opening.
Tenderness and pain occurs inside the vulva (lower lips) just at the opening of the vagina on the inside of the inner lips (labia minora). Some women have pain in one small area, while others have a more widespread involvement that can include areas all around the opening. 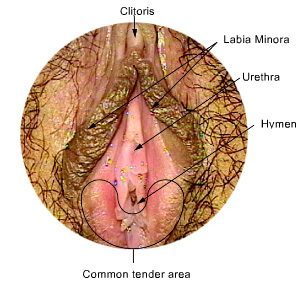 Imagine your vaginal opening as being round like a clock, the top part, below your clitoris and your urethra is at the 12 o’clock position and the bottom part of the vagina opening near your anus is at 6 o’clock .The most common tender areas are found between 5 o’clock and 7 o’clock. This area is associated with the tiny openings to the vestibular glands which provide lubrication, especially during sex. Pain in this area is called Vestibulodynia, while Vulvodynia can refer to pain anywhere on the vulva.
Imagine your vaginal opening as being round like a clock, the top part, below your clitoris and your urethra is at the 12 o’clock position and the bottom part of the vagina opening near your anus is at 6 o’clock .The most common tender areas are found between 5 o’clock and 7 o’clock. This area is associated with the tiny openings to the vestibular glands which provide lubrication, especially during sex. Pain in this area is called Vestibulodynia, while Vulvodynia can refer to pain anywhere on the vulva.
Other causes of pain or discomfort in your genital area
There are many other causes of pain in that area that can be treated quickly. These include the following:
- when you are not well lubricated and not ready for sex
- when you have hurt yourself during vigorous or unusual sex
- when you tear your vagina or vulva during sex
- when you have an infection or skin problem like a yeast infection, eczema, herpes and other skin changes,
- when your hymen and vaginal opening is too narrow
- when you have a skin infection from waxing or shaving
- women who are in menopause can also experience painful sex due to lack of estrogen causing dryness and irritation.
These are not Vestibulodynia and once treated or avoided do not cause longstanding pain.
How often does Vestibulodynia occur?
Up to 15% of women experience chronic or longstanding pain at the opening of the vagina. Because this is a sensitive and embarrassing topic, it is rarely discussed and many women suffer in silence until it gets very severe.
How does this affect you?
This pain can range from mild to excruciating and can eventually affect you and your relationship in many ways. Some women with Vulvodynia choose to remain single because of the pain. In essence, it’s frustrating and upsetting. It can impact your daily life, your sexuality and your emotional well-being. It is vital to realize that this affects women in different ways. Some women have very mild, occasional discomfort or pain, while others have severe, protracted pain which eventually affects their self-confidence, their sexual confidence, their relationships and sometimes causes depression. Everyone is different, so no matter how this affects you, we hope that you will be comfortable talking to us about it.
What happens when I have Vestibulodynia?
- The skin at the opening to your vagina gets sensitive and painful.
- This sometimes happens suddenly, but it usually gets worse over time, with episodes of no pain, and then suddenly flare-ups which can last a long time.
- Sex is painful when you or your partner puts a penis, vibrator, fingers, dildo or tongue against the sore area.
- This can get worse during thrusting, to the point where you cannot bear it any longer.
- “Please stop”: you may initially think silently, but by trying to be a participating partner, you sometimes bear the pain until it is too severe, then you have to stop, which can leave you feeling guilty although you are in pain. But it’s not your fault!
It is like someone has used sandpaper down there. The pain can last a long time, especially when you urinate after sex. Your vagina also reacts to protect you and can cause the vagina muscles to contract and undergo spasm, which causes you even more pain. Your vagina is sending a message. Don’t put anything in there please! This is called “Vaginismus “.
Let’s get talking!
- Many women find it difficult to talk about this sensitive issue.
- It goes to the core of who they are and being unable to feel and express this vital part of their life forces it underground.
- Some hide it and avoid talking about it.
- Sometimes women are taught not to talk about this area of their life.
- At Meridia Medical, we want to help you feel comfortable enough to seek the care you need.
We want you to get better.
We want women who have Vestibulodynia to feel supported and to know that this problem can be solved. It may take a while and the treatment may be multi-facetted and sometimes a matter of trial and error. Our goal is to find a solution tailored for you to get rid of the pain, and to equip you with coping strategies while we are involved in the treatment process. We would like to make it possible for you to be in charge of the pain to some degree, (rather that the pain controlling your actions and life) until the pain disappears. You wellness is our goal, not just the pain.
Have I done something wrong to cause this?
You can rest assured, that you have done nothing to bring this on. Unfortunately this just happens and it can happen to anyone.
Please never believe that this is your fault.
This pain is in your vaginal area, not in your head! The emotional effects of the pain are felt in your head and heart.
- It was not because you had a yeast infection,
- or that you are using the pill,
- or that you have Herpes,
- or that you may have slept with many partners,
- or that you had unusual sex.
- It is not because you are inexperienced! [This usually causes pain that does not stay long.]
Why does it happen?
You may not want to hear this, but we don’t really know what causes this painful scenario. There is much talk and debate in medical journals about it. Similar to many long standing pain problems, like Irritable Bowel, Interstitial Cystitis (painful bladder area) and atypical pelvic pain, we are not sure of the cause. It is likely due to a local skin change as well as a nerve and pain pathway problem. It is interesting that women who have Vestibulodynia sometimes have pain in other areas, or a more obvious response to painful stimulation. This makes us think that nerve pathways may also be implicated. This is not “nervous”, so never think that this is in your head. It is not! Some theoretical causes include a nonspecific inflammatory reaction, an autoimmune phenomenon (your body sometimes makes cells that affect other normal tissue), hormone causes, dietary intake (like oxalates), genetic causes and embryological causes (how the area is formed when you are developed in the womb). Even though we don’t know what the exact causes are, I recommend that you do not panic (Easy for me to say), because we can treat this You may have a yeast infection at the same time, but the likelihood of yeast causing this is small. There is no evidence that the latex from condoms causes this, but we do recommend that women stay clear of latex condoms and rather use polyurethane condoms (Avanti-made by Durex). Latex can sensitize the skin, and on the rare occasion can cause a severe allergic reaction.
Making the diagnosis?
The most important part to making a diagnosis it to listen to you. You have lived with this problem and we would like you to tell us about it:
- where it hurts,
- when it started,
- any coincidences,
- any other symptoms: (like bleeding, discharge, pain with tampons, pain with sex, no lubrication during sex, no libido or sex drive),
- avoiding your partner and sex,
- feeling depressed,
- other painful areas.
Hearing you tell your story is the most important part of making the diagnosis and treating you. Your information will help us decide what medications to use and what to avoid.
The Examination
We do a very gentle examination with you in charge every step of the way. At Meridia Gynecology, we know that this is a very sensitive, intrusive and vulnerable time for you. We understand that you may have had unpleasant examinations and experiences in the past or perhaps had sexual trauma or abuse. We respect you and want you to feel safe and cared for. Please read our information: “Your Gyne Examination“. We don’t just talk; we go out of our way to help you. We examine all the areas if possible, and only if you feel comfortable. During the examination we identify your anatomy with you. We use a viewing monitor to have you help us identify areas that hurt or irritate you. We always use a Colposcope to examine the area. This is nothing more than a camera microscope that enlarges the area so that we can see more clearly and identify any small changes that we cannot see with our naked eyes. This also makes it possible for you to see on the viewing monitor what we are seeing, if you are comfortable looking. We hope that you will get past the natural shyness and embarrassment and see your genital area as you would do when examining your hands or face. (yes, for real!) This also gives you the opportunity to ask those difficult questions you have always wanted to ask. This is the time that we can show you how we can help treat the area. We encourage you to be in charge of your vagina / vulva area, and to help with the management and to enjoy all the other wondrous aspects of that part of your body, if you wish. We may also do tests of the discharge or cells of the skin. This is not painful, except for the tenderness that you already have.
What now? Treatment:
We want you to know that we can help you and with time and patience, you will overcome this. There are many treatments we can use and we will find the combination that helps you best.
Treatments we use at Meridia Gynecology
We cannot stress enough, the importance of helping you cope with the situation. Some women are depressed about this and we will help treat this as well. If you are having difficulty coping with the situation and finding that you are feeling depressed or unable to focus on your day to day life, we will help you find help. This could be a cognitive therapist, a sexual medicine therapist, a psychiatrist or a social worker. Please see our “˜Vulva Care Guide’. This is a list of helpful ideas to protect your genital skin and prevent irritation. It also reviews lubrication and newer types of condoms.
Topical creams and ointments:
- We get best results with a compounded combination of Estriol, Clotrimazole and steroid ointment.
Other options:
- Topical Lidocaine (2% viscous) numbs the area, This may decrease pain if used overnight for a few weeks. Lidocaine is great when you are at a stage in treatment when you are considering biofeedback and perhaps intercourse, or with mild to moderate initial pain.
- Topical Amitryptaline and Baclofen: This ointment is compounded for us. The problem is finding the correct base cream. Most have alcohol or preservatives which aggravate the pain and burning. Aquaphor seems to be a good vehicle for most women.
- Estrogen cream, either bioidentical or Premarin. I generally use this in combination with Progesterone. This seems to have a good effect when it works, especially in women >45.
- Clotrimazole ointment, although not found to be supported in the literature, works anecdotally for many women. I attribute its benefit to the anti-inflammatory properties
- Gabapentin applied topically.
Topical Medicines that we do not use because we find them ineffective: Cromolyn cream.
Oral Medications:
This depends on the situation, involvement of Depression and other pain issues.
Neuromodulators:These drugs work at the level of the nerve pathways and the brain. They likely modify the pain response and can be very helpful.
|
Cognitive Therapy
This is a type of psychotherapy (mental, rather than physical therapy) which helps you manage your pain. We are not saying for a moment that the pain is in your mind. However, your response to pain and your mental approach has been found in studies to be most helpful in decreasing pain This type of therapy just provides you with the mental tools to help while we use all the other options. Some women catastophize the pain due to the constant nature of the pain and the dread of experiencing it when you have sex, exercise, sit etc. Cognitive therapy can help you manage this aspect as well.
Acupuncture
This can be helpful and I recommend it once a general approach has been instituted. The reason that I do not start with it, is because I want it to be successful. I have found acupuncture to be helpful once other aspects have been identified and managed.
Biofeedback
We use biofeedback as our standard treatment foundation. We designed soft vaginal dildo’s, in 5 sizes in addition to a vibrator attachment. [These can he purchased from us without a gynecological consultation.] This has many benefits:
- Desensitizes the area over time
- Gives you back control of you vulva and vagina
- Helps relax the vaginal muscles if they are in spasm
- Allows you to be in complete control of vaginal penetration, until you have vaginal intercourse
- The vibrator attachment helps decrease pain sensation. Vibration sense can desensitize the area of pain, without affecting sexual enjoyment later.
- ….and it can be fun.
Low Oxalate Diet
- Oxalate can sometime irritate the area. Using a low Oxalate diet and Calcium Citrate can help, but rarely used..
Surgery:
- At Merida Gynecology, we will always first use other options and try our best to avoid surgery. However, if other treatment is clearly not working, surgery is better than you experiencing pain for too long.
- We try to focus on how you are doing rather than try multiple modalities without success for too long. This is when surgery is a good option.
- The procedure is tailored to the area affected. Today, this procedure (called Vestibulectomy) can safely be done using local anaesthesia, without the need for a general anaesthetic. At Merida Gynecology, we use a CO2 Ultrapulse laser to remove the sensitive tissue before repositioning the surrounding skin over the area that was removed. This has a very good result.
Buyer Beware!
There are many treatments out there that are advertised as the cure. When you are in pain, feeling vulnerable and frustrated, it is easy to grab anything you see on the internet or hear about from other people. Please be safe and know what you are using. Find a doctor that you trust, who can listen and who has an open mind to new treatments. Discuss your options before trying out any treatment that may be ineffective or have harmful side effects. . Please don’t harm yourself or set yourself up for failure.
SEX: [ Black box warning!]
Vaginal intercourse does not make the pain get better. It makes it worse, and each time that happens you feel poorly and guilty, ever though this is not your fault. Never let someone tell you to have sex to “end” to the pain. If you have a partner, it is very helpful for your partner to participate in and understand your treatment. This will help you feel supported and less pressured to “perform” vaginal sex. You don’t have to put your sexuality on hold. It just has to be modified until the pain is better.
No vaginal penetration until the pain is better.
That can take a few months! This means no penis, tampon or sex toys in your vagina! However, we recommend that you enjoy and participate in other types of sex if you wish. If you are comfortable masturbating or having oral sex, please do so. This will reconnect you with your normal sexuality and help you feel better. Pleasure decreases the sensation of pain. (Endorphin effect) Talking to a sex therapist or if you are in a relationship, a couple’s sex therapist may be very helpful.
We need your help!
Please feel welcome and safe in telling us about this malady that affects up to 15% of women. We will work with you to achieve success. You are the most important predictor of your success and we need you to understand and participate in your treatment.
Wishing you success
Links to other sites that will be helpful: NATIONAL VULVODYNIA ASSOCIATION: www.nva.org INTERNATIONAL SOCIETY FOR THE STUDY OF VULVOVAGINAL DISEASE (ISSVD): www.issvd.org
